S666 là một trong những nhà cái cá cược trực tuyến nổi tiếng hàng đầu tại châu Á, thu hút đông đảo người chơi bởi sự đa dạng về sản phẩm, dịch vụ chất lượng và uy tín đã được khẳng định. Bài viết này sẽ đi sâu vào phân tích những yếu tố làm nên thành công của S666, khám phá những ưu điểm nổi bật và đánh giá tiềm năng phát triển của nhà cái này trong tương lai.
S666 – Giấy chứng nhận uy tín và hành lang pháp lý vững chắc
Nhà cái S666 xây dựng uy tín dựa trên nền tảng pháp lý vững chắc, đảm bảo môi trường cá cược an toàn và minh bạch cho người chơi.
Trước khi H3 tag write paragraph : Việc hiểu rõ về nguồn gốc pháp lý và các giấy chứng nhận hoạt động của S666 là vô cùng quan trọng. Điều này giúp người chơi yên tâm hơn khi tham gia cá cược và tin tưởng vào sự công bằng, minh bạch của nhà cái.
Giấy phép hoạt động hợp pháp
S666 sở hữu giấy phép hoạt động hợp pháp được cấp bởi các tổ chức uy tín trong ngành cá cược. Điều này chứng minh rằng nhà cái đã đáp ứng đầy đủ các tiêu chuẩn về an ninh, tài chính và công bằng, đồng thời chịu sự giám sát chặt chẽ của các cơ quan quản lý. Việc có giấy phép hoạt động hợp pháp không chỉ là minh chứng cho sự uy tín mà còn đảm bảo quyền lợi của người chơi trong trường hợp có tranh chấp xảy ra.
Các tổ chức cấp phép thường xuyên kiểm tra và đánh giá hoạt động của S666 để đảm bảo tuân thủ các quy định và tiêu chuẩn quốc tế. Do đó, người chơi có thể hoàn toàn tin tưởng vào sự an toàn và minh bạch khi tham gia cá cược tại đây. S666 luôn đặt sự uy tín lên hàng đầu, và việc có giấy phép hoạt động hợp pháp là một trong những cam kết mạnh mẽ nhất của nhà cái đối với người chơi.
Tôi cho rằng, việc S666 công khai thông tin về giấy phép hoạt động trên trang web của mình là một hành động thể hiện sự minh bạch và chuyên nghiệp. Người chơi có thể dễ dàng kiểm tra và xác minh tính hợp lệ của giấy phép, từ đó cảm thấy an tâm và tin tưởng hơn khi tham gia cá cược.
Cam kết bảo mật thông tin cá nhân
S666 hiểu rõ tầm quan trọng của việc bảo mật thông tin cá nhân của người chơi. Vì vậy, nhà cái đã đầu tư mạnh mẽ vào hệ thống bảo mật tiên tiến, sử dụng các công nghệ mã hóa hiện đại để bảo vệ dữ liệu khỏi các cuộc tấn công mạng. Thông tin cá nhân của người chơi được lưu trữ trên các máy chủ an toàn, được bảo vệ bằng nhiều lớp bảo mật.
Ngoài ra, S666 còn có chính sách bảo mật rõ ràng, quy định về việc thu thập, sử dụng và chia sẻ thông tin cá nhân của người chơi. Nhà cái cam kết không tiết lộ thông tin cá nhân của người chơi cho bất kỳ bên thứ ba nào trừ khi có yêu cầu của pháp luật. Chính sách bảo mật này giúp người chơi cảm thấy yên tâm khi cung cấp thông tin cá nhân cho S666.
Theo kinh nghiệm của tôi, việc đọc kỹ chính sách bảo mật của nhà cái trước khi đăng ký tài khoản là vô cùng quan trọng. Điều này giúp bạn hiểu rõ về cách nhà cái bảo vệ thông tin cá nhân của bạn và đảm bảo quyền lợi của mình. S666 là một trong số ít các nhà cái cung cấp chính sách bảo mật chi tiết và dễ hiểu, thể hiện sự tôn trọng đối với người chơi.
Cơ chế giải quyết tranh chấp công bằng
S666 xây dựng một cơ chế giải quyết tranh chấp công bằng, minh bạch, đảm bảo quyền lợi của cả người chơi và nhà cái. Khi có tranh chấp xảy ra, người chơi có thể liên hệ với bộ phận hỗ trợ khách hàng của S666 để được giải quyết. Nhà cái sẽ xem xét kỹ lưỡng các bằng chứng và đưa ra quyết định dựa trên các quy định và điều khoản đã được công bố.
Trong trường hợp người chơi không đồng ý với quyết định của S666, họ có thể khiếu nại lên các tổ chức quản lý cá cược để được giải quyết. S666 luôn sẵn sàng hợp tác với các tổ chức này để đảm bảo tính công bằng và minh bạch trong quá trình giải quyết tranh chấp. Cơ chế giải quyết tranh chấp này giúp người chơi cảm thấy an tâm khi tham gia cá cược tại S666, biết rằng quyền lợi của mình sẽ được bảo vệ.
Tôi đánh giá cao việc S666 có một cơ chế giải quyết tranh chấp rõ ràng và minh bạch. Điều này cho thấy nhà cái luôn coi trọng quyền lợi của người chơi và sẵn sàng giải quyết các vấn đề một cách công bằng. Đây là một yếu tố quan trọng giúp S666 xây dựng uy tín và lòng tin của người chơi.
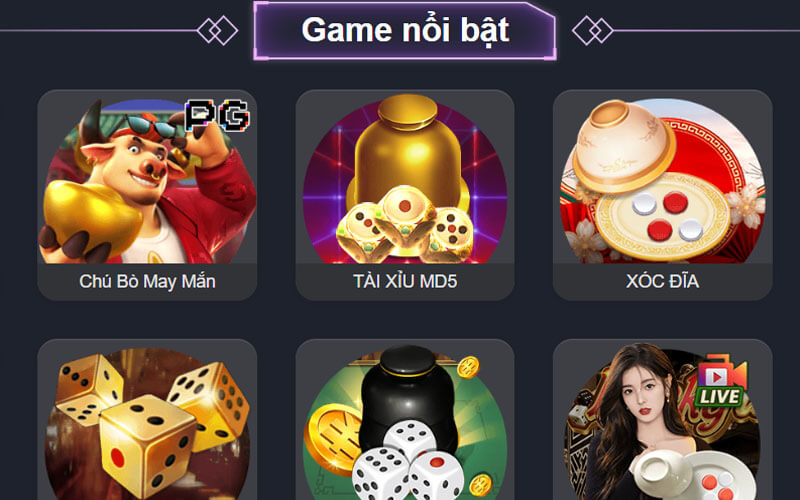
Kho game đa dạng và hấp dẫn tại S666
Nhà cái S666 nổi tiếng với kho game cá cược đa dạng và hấp dẫn, đáp ứng mọi nhu cầu giải trí của người chơi.
Trước khi H3 tag write paragraph : Sự đa dạng về trò chơi là một trong những yếu tố quan trọng nhất thu hút người chơi đến với S666. Từ cá cược thể thao đến casino trực tuyến, từ slot game đến xổ số, người chơi có thể tìm thấy mọi trò chơi yêu thích tại đây.
Cá cược thể thao đỉnh cao
S666 cung cấp một nền tảng cá cược thể thao đỉnh cao với hàng ngàn sự kiện thể thao mỗi ngày. Người chơi có thể cá cược vào các môn thể thao phổ biến như bóng đá, bóng rổ, tennis, cầu lông, bóng chuyền, và nhiều môn thể thao khác. S666 cung cấp đa dạng các loại kèo cược, từ kèo châu Á, kèo châu Âu, kèo tài xỉu đến kèo rung, kèo tỷ số, đáp ứng mọi sở thích của người chơi.
Tỷ lệ kèo cược tại S666 được đánh giá là cạnh tranh so với các nhà cái khác trên thị trường. Nhà cái thường xuyên cập nhật tỷ lệ kèo cược để đảm bảo người chơi có được những lựa chọn tốt nhất. Ngoài ra, S666 còn cung cấp các thông tin thống kê, phân tích chuyên sâu về các trận đấu, giúp người chơi có thể đưa ra những quyết định cá cược chính xác hơn.
Tôi nhận thấy rằng, S666 không chỉ là một nhà cái cá cược thể thao mà còn là một nguồn thông tin thể thao hữu ích cho người chơi. Các bài viết phân tích, nhận định về các trận đấu được đăng tải thường xuyên trên trang web của S666 giúp người chơi có cái nhìn toàn diện và sâu sắc hơn về các sự kiện thể thao.
Casino trực tuyến sống động
S666 mang đến cho người chơi trải nghiệm casino trực tuyến sống động như đang ở trong một sòng bài thực thụ. Nhà cái hợp tác với các nhà cung cấp game casino hàng đầu thế giới như Evolution Gaming, Pragmatic Play, Microgaming, để cung cấp các trò chơi casino chất lượng cao với đồ họa sắc nét, âm thanh sống động và dealer chuyên nghiệp.
Người chơi có thể tham gia các trò chơi casino phổ biến như Baccarat, Blackjack, Roulette, Sicbo, Poker, và nhiều trò chơi khác. S666 cung cấp nhiều phiên bản khác nhau của mỗi trò chơi, đáp ứng mọi sở thích và trình độ của người chơi. Đặc biệt, S666 còn có các bàn chơi casino trực tuyến với người chia bài thật, mang đến cho người chơi trải nghiệm chân thực và hấp dẫn.
Theo quan điểm của tôi, casino trực tuyến tại S666 là một lựa chọn tuyệt vời cho những người yêu thích các trò chơi casino nhưng không có điều kiện đến các sòng bài thực thụ. Với sự đa dạng về trò chơi, chất lượng đồ họa và âm thanh tuyệt vời, và đội ngũ dealer chuyên nghiệp, S666 mang đến cho người chơi những trải nghiệm casino trực tuyến không thể nào quên.
Slot game đa dạng chủ đề
S666 sở hữu một bộ sưu tập slot game khổng lồ với hàng trăm trò chơi khác nhau. Các trò chơi slot game tại S666 được thiết kế với đồ họa đẹp mắt, âm thanh sống động và nhiều chủ đề khác nhau, từ cổ điển đến hiện đại, từ phiêu lưu đến thần thoại. Người chơi có thể dễ dàng tìm thấy trò chơi slot game yêu thích của mình tại S666.
S666 thường xuyên cập nhật các trò chơi slot game mới nhất, đảm bảo người chơi luôn có những trải nghiệm mới mẻ và thú vị. Các trò chơi slot game tại S666 có tỷ lệ trả thưởng cao, mang đến cho người chơi cơ hội giành được những phần thưởng lớn. Ngoài ra, S666 còn có các chương trình khuyến mãi hấp dẫn dành cho người chơi slot game, giúp người chơi tăng cơ hội chiến thắng.
Tôi tin rằng, slot game là một trong những sản phẩm chủ lực của S666. Với sự đa dạng về chủ đề, đồ họa đẹp mắt, âm thanh sống động và tỷ lệ trả thưởng cao, slot game tại S666 luôn thu hút đông đảo người chơi tham gia. S666 cũng thường xuyên tổ chức các giải đấu slot game với những phần thưởng hấp dẫn, tạo thêm sự hứng thú cho người chơi.
Giao diện thân thiện và trải nghiệm người dùng tối ưu
Nhà cái S666 chú trọng đến việc xây dựng một giao diện thân thiện và tối ưu hóa trải nghiệm người dùng.
Trước khi H3 tag write paragraph : Giao diện người dùng là yếu tố đầu tiên mà người chơi tiếp xúc khi truy cập vào trang web của S666. Một giao diện thân thiện, dễ sử dụng sẽ giúp người chơi dễ dàng tìm kiếm thông tin, tham gia cá cược và tận hưởng các dịch vụ của nhà cái.
Thiết kế trực quan và dễ sử dụng
Giao diện của S666 được thiết kế trực quan, logic, với màu sắc hài hòa và bố cục rõ ràng. Người chơi có thể dễ dàng tìm thấy các trò chơi, sự kiện thể thao, chương trình khuyến mãi và các thông tin khác mà mình cần. Các nút chức năng được thiết kế lớn, dễ nhìn, giúp người chơi thao tác dễ dàng trên cả máy tính và thiết bị di động.
S666 cũng hỗ trợ nhiều ngôn ngữ khác nhau, giúp người chơi từ nhiều quốc gia có thể sử dụng trang web một cách dễ dàng. Trang web của S666 được tối ưu hóa để tải nhanh, không gây giật lag, đảm bảo người chơi có trải nghiệm mượt mà và không bị gián đoạn khi tham gia cá cược.
Theo đánh giá của tôi, giao diện của S666 là một trong những giao diện tốt nhất trên thị trường cá cược trực tuyến hiện nay. Sự đơn giản, trực quan và dễ sử dụng của giao diện giúp S666 thu hút được nhiều người chơi, đặc biệt là những người mới bắt đầu tham gia cá cược trực tuyến.
Tương thích đa nền tảng
S666 không chỉ có giao diện web mà còn phát triển ứng dụng di động cho cả hệ điều hành iOS và Android. Ứng dụng di động của S666 có đầy đủ các tính năng như giao diện web, cho phép người chơi tham gia cá cược mọi lúc mọi nơi, chỉ cần có kết nối internet. Ứng dụng di động của S666 được thiết kế tối ưu cho các thiết bị di động, đảm bảo người chơi có trải nghiệm tốt nhất trên điện thoại và máy tính bảng.
Với ứng dụng di động của S666, người chơi có thể dễ dàng theo dõi các trận đấu thể thao trực tiếp, nhận thông báo về các chương trình khuyến mãi và rút tiền một cách nhanh chóng. Ứng dụng di động của S666 là một công cụ hữu ích cho những người chơi thường xuyên di chuyển và muốn tham gia cá cược mọi lúc mọi nơi.
Tôi nhận thấy rằng, việc S666 phát triển ứng dụng di động cho thấy nhà cái rất quan tâm đến trải nghiệm của người dùng. Ứng dụng di động giúp S666 tiếp cận được nhiều người chơi hơn và cung cấp cho người chơi sự tiện lợi tối đa khi tham gia cá cược.
Hỗ trợ khách hàng chuyên nghiệp 24/7
S666 có đội ngũ hỗ trợ khách hàng chuyên nghiệp, nhiệt tình và sẵn sàng giải đáp mọi thắc mắc của người chơi 24/7. Người chơi có thể liên hệ với bộ phận hỗ trợ khách hàng của S666 thông qua nhiều kênh khác nhau như chat trực tuyến, email, điện thoại, và các mạng xã hội.
Đội ngũ hỗ trợ khách hàng của S666 được đào tạo bài bản, có kiến thức chuyên sâu về các sản phẩm và dịch vụ của nhà cái. Họ có thể giải đáp mọi thắc mắc của người chơi một cách nhanh chóng và chính xác. S666 luôn đặt sự hài lòng của khách hàng lên hàng đầu, và đội ngũ hỗ trợ khách hàng là một trong những yếu tố quan trọng giúp S666 đạt được mục tiêu này.
Theo kinh nghiệm của tôi, dịch vụ hỗ trợ khách hàng là một trong những yếu tố quan trọng nhất để đánh giá chất lượng của một nhà cái. S666 đã làm rất tốt trong lĩnh vực này. Đội ngũ hỗ trợ khách hàng của S666 luôn sẵn sàng giúp đỡ người chơi và giải quyết các vấn đề một cách nhanh chóng và hiệu quả.
Các chương trình khuyến mãi và ưu đãi hấp dẫn tại S666
Nhà cái S666 thường xuyên tung ra các chương trình khuyến mãi và ưu đãi hấp dẫn, thu hút người chơi mới và tri ân người chơi cũ.
Trước khi H3 tag write paragraph : Khuyến mãi là một phần không thể thiếu trong chiến lược thu hút và giữ chân người chơi của các nhà cái. S666 hiểu rõ điều này và luôn cố gắng mang đến cho người chơi những chương trình khuyến mãi hấp dẫn và giá trị nhất.
Khuyến mãi chào mừng thành viên mới
S666 có chương trình khuyến mãi chào mừng thành viên mới vô cùng hấp dẫn. Người chơi mới khi đăng ký tài khoản và thực hiện gửi tiền lần đầu sẽ được nhận một khoản tiền thưởng lớn. Khoản tiền thưởng này có thể được sử dụng để tham gia cá cược vào các trò chơi khác nhau tại S666.
Ngoài ra, S666 còn có các chương trình khuyến mãi khác dành cho thành viên mới như tặng vòng quay miễn phí, hoàn trả tiền cược, và nhiều ưu đãi khác. Các chương trình khuyến mãi này giúp người chơi mới có cơ hội trải nghiệm các sản phẩm và dịch vụ của S666 một cách dễ dàng và tiết kiệm.
Từ góc độ của một người chơi, tôi thấy các chương trình khuyến mãi chào mừng thành viên mới của S666 rất hấp dẫn và có giá trị. Chúng giúp người chơi mới có thêm vốn để tham gia cá cược và khám phá các trò chơi khác nhau tại S666.
Khuyến mãi hoàn trả tiền cược
S666 có chương trình khuyến mãi hoàn trả tiền cược hàng tuần, hàng tháng, giúp người chơi giảm thiểu rủi ro khi tham gia cá cược. Tỷ lệ hoàn trả tiền cược có thể lên đến vài phần trăm, tùy thuộc vào cấp độ thành viên và loại trò chơi mà người chơi tham gia.
Chương trình khuyến mãi hoàn trả tiền cược là một trong những chương trình khuyến mãi được yêu thích nhất tại S666. Nó giúp người chơi có thêm động lực để tham gia cá cược và giảm bớt áp lực khi gặp phải những ván cược không thành công.
Theo tôi, chương trình khuyến mãi hoàn trả tiền cược của S666 là một chương trình khuyến mãi rất thiết thực và có lợi cho người chơi. Nó giúp người chơi có thể chơi lâu hơn và có nhiều cơ hội chiến thắng hơn.
Các chương trình khuyến mãi đặc biệt
S666 thường xuyên tổ chức các chương trình khuyến mãi đặc biệt vào các dịp lễ, Tết, sự kiện thể thao lớn, và các dịp đặc biệt khác. Các chương trình khuyến mãi này có thể bao gồm tặng tiền thưởng, tặng quà, tặng vòng quay miễn phí, hoàn trả tiền cược, và nhiều ưu đãi khác.
Các chương trình khuyến mãi đặc biệt của S666 thường có giá trị rất lớn và thu hút đông đảo người chơi tham gia. Chúng tạo thêm sự hứng thú và kịch tính cho người chơi khi tham gia cá cược tại S666.
Tôi đánh giá cao việc S666 thường xuyên tổ chức các chương trình khuyến mãi đặc biệt. Điều này cho thấy nhà cái luôn quan tâm đến người chơi và muốn mang đến cho người chơi những trải nghiệm tốt nhất.
S666 – Cộng đồng người chơi lớn mạnh và tích cực
Nhà cái S666 đã xây dựng được một cộng đồng người chơi lớn mạnh và tích cực.
Trước khi H3 tag write paragraph : Một cộng đồng người chơi lớn mạnh và tích cực là một yếu tố quan trọng giúp một nhà cái phát triển bền vững. S666 đã thành công trong việc xây dựng một cộng đồng như vậy.
Diễn đàn và các nhóm thảo luận trực tuyến
S666 có diễn đàn và các nhóm thảo luận trực tuyến, nơi người chơi có thể giao lưu, chia sẻ kinh nghiệm, hỏi đáp thắc mắc, và thảo luận về các vấn đề liên quan đến cá cược. Diễn đàn và các nhóm thảo luận trực tuyến là nơi người chơi có thể kết nối với những người có cùng sở thích và niềm đam mê. Nhờ đó, người chơi cảm thấy không đơn độc và có thêm động lực để tham gia cá cược.
S666 cũng thường xuyên tổ chức các sự kiện, minigame, và giải đấu trong diễn đàn và các nhóm thảo luận trực tuyến, tạo thêm sự hứng thú và gắn kết cho cộng đồng người chơi.
Tôi thấy rằng, diễn đàn và các nhóm thảo luận trực tuyến là một phần quan trọng của cộng đồng người chơi S666. Chúng là nơi người chơi có thể học hỏi, chia sẻ, và giúp đỡ lẫn nhau.
Sự kiện offline và gặp mặt người chơi
S666 đôi khi tổ chức các sự kiện offline và gặp mặt người chơi tại các thành phố lớn. Các sự kiện này là cơ hội để người chơi gặp gỡ, giao lưu, và chia sẻ kinh nghiệm trực tiếp với nhau. Các sự kiện offline và gặp mặt người chơi thường được tổ chức với quy mô lớn, có sự tham gia của các thành viên ban quản lý S666, các chuyên gia cá cược, và các người chơi nổi tiếng trong cộng đồng.
Các sự kiện offline và gặp mặt người chơi giúp S666 xây dựng mối quan hệ tốt đẹp với người chơi và tạo ra một cộng đồng gắn kết.
Theo quan điểm của tôi, việc S666 tổ chức các sự kiện offline và gặp mặt người chơi là một hành động rất ý nghĩa. Nó cho thấy nhà cái rất quan tâm đến người chơi và muốn xây dựng một cộng đồng vững mạnh.
Chương trình VIP và tri ân khách hàng thân thiết
S666 có chương trình VIP và tri ân khách hàng thân thiết với nhiều ưu đãi đặc biệt như tặng tiền thưởng, tặng quà, hoàn trả tiền cược, và nhiều ưu đãi khác. Các thành viên VIP của S666 còn được hưởng các dịch vụ hỗ trợ khách hàng ưu tiên và được tham gia các sự kiện đặc biệt dành riêng cho thành viên VIP.
Chương trình VIP và tri ân khách hàng thân thiết là một cách để S666 thể hiện sự trân trọng đối với những người chơi đã gắn bó lâu dài với nhà cái. Nó cũng là một động lực để người chơi tiếp tục ủng hộ và tin tưởng vào S666.
Tôi tin rằng, chương trình VIP và tri ân khách hàng thân thiết của S666 là một chương trình rất tốt và có lợi cho người chơi. Nó giúp người chơi cảm thấy được trân trọng và có thêm động lực để tham gia cá cược.
Kết luận
S666 nổi bật lên như một nhà cái hàng đầu châu Á, đạt được thành công nhờ vào nền tảng pháp lý vững chắc, kho game đa dạng và hấp dẫn, giao diện người dùng thân thiện, các chương trình khuyến mãi hấp dẫn, và cộng đồng người chơi lớn mạnh. Những yếu tố này đã giúp S666 xây dựng được uy tín và lòng tin của người chơi, đồng thời tạo đà cho sự phát triển bền vững trong tương lai.